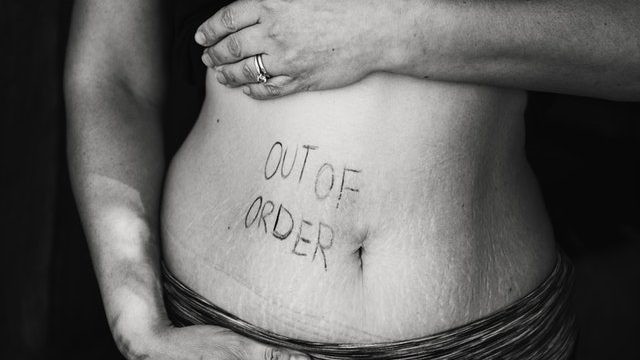
Epilepsy and its treatment affect all life stages of women. Epilepsy brings special issues for women, particularly during epilepsy in pregnancy.
Pregnancy impacts epilepsy and epilepsy impacts pregnancy. Nevertheless over 90% of women with epilepsy who become pregnant have healthy babies.
Seizures In Pregnancy
During pregnancy, the frequency of seizures declines or remains the same in most women. In about 20% to 30% of women, there may be an increase in seizure frequency, mainly in the first or third trimester. The increased seizure frequency does not depend on the type or duration of seizures the woman has or even the presence of seizures in a previous pregnancy.
The possible triggers for these seizures are:
- Hormone changes
- Water and Sodium Retention
- Stress
- Decreasing Blood Levels of Antiepileptic Medications.
- Voluntary stopping the medication is amongst the commonest reason for the seizure.
Women who are seizure-free for the last one year, have a high chance of being seizure-free during pregnancy.
Generalized seizures are a big risk to the mother and the baby such as trauma from falls and burns, preterm labor, and miscarriage.
Focal seizures are not as risky compared to generalized ones.
Management With Respect To Pregnancy
Planned pregnancies are usually best for women with epilepsy.
It is important to have a neurology/epilepsy team and an obstetrical team who will work jointly.
One must get the seizures under control, take the right medications at the right dose, and try to reduce the medication to the bare minimum.
Anti-epileptic drugs (AEDs) can cause congenital malformation or birth defects but one must continue the medication.
Risks from seizures in the mother during pregnancy are greater than the risks from seizure medications.
The lowest possible dose of seizure medication that will control seizures is recommended.
Being on a single drug will decrease the risk of birth defects and result in fewer drug interactions, fewer side effects, and improve compliance.
In the general population, there is a 2% to 3% occurrence of congenital malformations but in women with epilepsy, the risk is doubled to about 4% to 6%. The most common malformations include cleft lip and cleft palate and cardiac defects.
Valproate or valproic acid (VPA) is a commonly used drug and increases the risk of neural tube defects (lack of spinal cord closure) in newborns. Also, there is an increased risk of developing a baby having behavioral impairments later in life, such as lower IQ, and autism disorders. Therefore, it is avoided in women who are planning a pregnancy.
All women with epilepsy are advised to take a daily multivitamin containing 0.4 mg folate, and an additional 4-mg folate supplement. Selenium and zinc present in the multivitamin tablet are useful.
Monitoring drug levels is particularly important. Antiepileptic drug levels should be checked during the pregnancy and following delivery. The levels of AEDs decline during pregnancy due to an increase in blood volume and therefore dosage adjustments may be needed. Monitoring in the post-partum period is also needed as levels rise postdelivery.
Every woman must be counseled for first and second-trimester screening methods available and a high resolution or level II ultrasound to detect birth defects.
Epilepsy does not influence the mode of delivery and is not an indication for a cesarean section. Most women will deliver normally, and caesareans may be required for obstetric reasons alone.
Children born to women taking antiepileptics should be given vitamin K at the time of birth to prevent rare bleeding complications.
Breastfeeding is generally safe and recommended for its important benefits to the infant.
Have more questions about Epilepsy In Pregnancy or Need help with managing it. Get an appointment with Dr. Sangeeta Agrawal